
There is a separate out-of-pocket maximum for in-network prescriptions. In general, Tier 1 is generic drugs, Tier 2 is preferred brand drugs, and Tier 3 includes non-preferred drugs. Retail and mail order prescription copays are based on a tiered drug list. These copays do not apply towards the plan’s medical deductible, coinsurance, or out-of-pocket maximum. The $500 Deductible plan has set copays for prescriptions.
#COPAY AFTER DEDUCTIBLE DOWNLOAD#
Download the list of preventive medications or contact CVS Caremark directly at 1-86. For those preventive prescriptions, you only pay the 20% coinsurance. $2,400 per individual / $7,200 family maximumįor all medical plans, there are some prescriptions that are covered by the plan at 100%, as defined by the Affordable Care Act (ACA).įor the HDHP, there are additional preventive medications that are allowed to bypass the deductible and are subject only to coinsurance.$3,600 for employee only coverage / $7,200 all other coverage levels.When the deductible and coinsurance amounts that you’ve paid equal the plan’s out-of-pocket maximum then the plan pays 100% of covered charges for the remainder of the plan year.
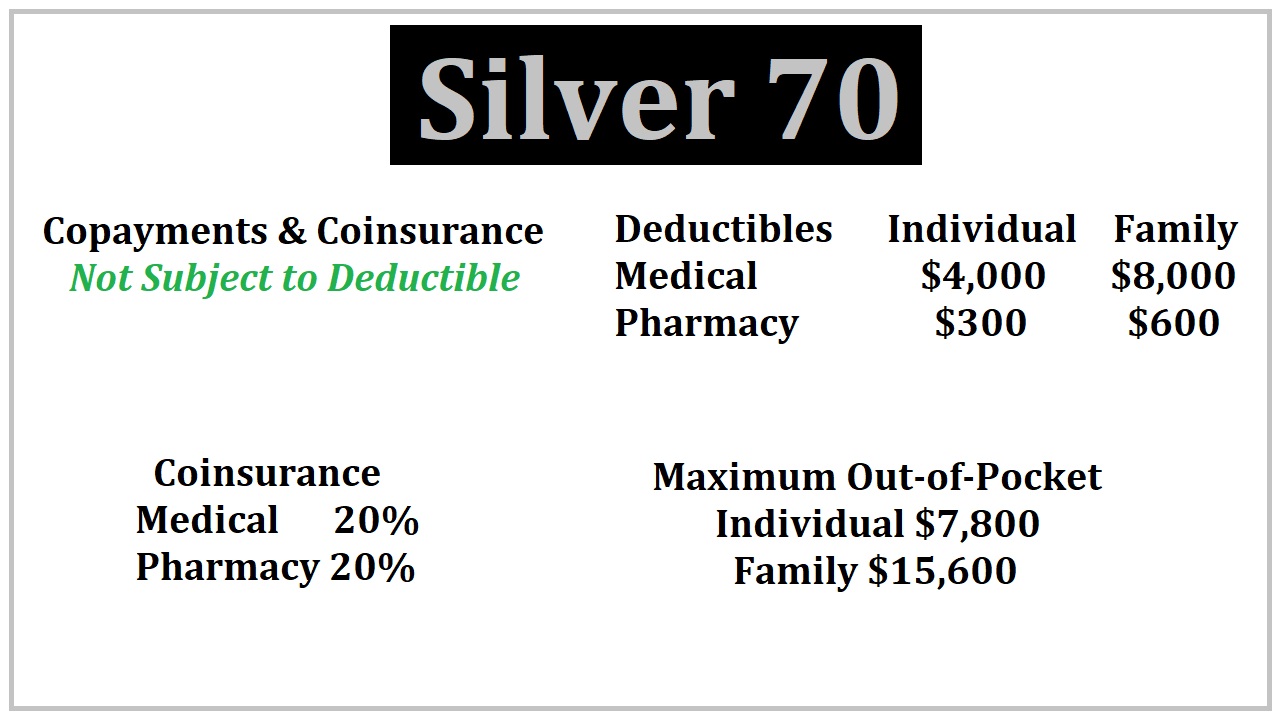
The Out-of-Pocket Maximum protects you from high medical bills. There is a completely separate deductible and coinsurance rate for both Anthem plans when out-of-network providers are used. You will continue to pay this amount until your out-of-pocket costs reach the annual out-of-pocket maximum. That means you will pay 20 percent and the plan will pay 80 percent of the costs for in-network services once the deductible has been met. Each of IU’s medical plans has your share of the coinsurance for in-network care set at 20%. In addition to a deductible, health insurance also has coinsurance. Coinsurance is the percentage of the costs that you share with the plan once you have met your deductible. Each enrollee may contribute no more than the amount of the individual deductible to the family deductible.If the family deductible is met, the plan begins to pay its share of the cost of healthcare expenses for all members of the family whether or not they’ve met their own individual deductibles.If an individual meets his or her individual deductible, the plan begins to pay its share of the cost of healthcare expenses for that individual only, but not for the other family members.There are two ways the plan will begin to pay its share of the cost of healthcare expenses for a particular individual within the family.As medical expenses are incurred, the amount each family member pays toward these expenses is credited to their individual deductible and to the family deductible.




 0 kommentar(er)
0 kommentar(er)
